Author:
Clinically Reviewed By:
Many people exploring weight loss surgery are looking for clarity, support, and a clear path forward, and we’ve seen how helpful it can be to understand the full picture before making a decision. As Registered Dietitians, we’ve spent years helping patients navigate the options, the benefits, the risks, and the long-term commitments involved.
This article walks through what weight loss surgery is, the different procedures available, how much weight people typically lose, who qualifies, how much it costs, and what to expect during preparation and recovery.
We also cover special situations, comparisons with medication-based treatments, and how to choose a high-quality surgical program. Our goal is to give you practical, honest information so you can feel confident taking your next step.
What Is Weight Loss Surgery?
Weight loss surgery is a medical treatment that changes how the stomach or intestines work to support meaningful and lasting weight reduction. Many people think of it as a procedure that simply makes the stomach smaller, but there’s more happening inside the body.
These surgeries also influence hunger hormones, how quickly food moves through the digestive system, and how the body processes blood sugar. That combination often leads to stronger metabolic improvements than people see with lifestyle changes alone.
The term metabolic and bariatric surgery reflects this broader impact. For example, some procedures reduce stomach size to help you feel full sooner, while others adjust the path food takes through the intestines. These changes can improve conditions like type 2 diabetes, high blood pressure, or sleep apnea, which often accompany higher body weight.
Weight loss surgery is considered when someone is diagnosed with Class III obesity or Class II obesity with another medical diagnosis. It’s also an option for people who have tried structured diets, increased physical activity, and long-term habit changes but still struggle to lose weight or keep it off.
From our experience as Registered Dietitians, surgery works best when paired with strong nutrition support, behavior change, and long-term follow-up. It’s a tool with real medical power, and for many people it can support better health and an easier daily routine.
If you want guidance that feels clear and personal, connect with a Registered Bariatric Dietitian to get support through the process.

Types of Weight Loss Surgery (and How They Work)
Understanding the different procedures helps you picture what each option can offer and what the long-term commitment looks like. Some surgeries focus on restriction, others influence metabolism, and some do both at once. Each has its own benefits and challenges.
Sleeve Gastrectomy (VSG)
A sleeve gastrectomy removes most of the stomach and leaves a narrow, tube-shaped pouch behind. That smaller stomach helps you feel full with less food, and many people also notice a real change in hunger because the procedure reduces certain appetite hormones. The process is straightforward and tends to appeal to people who want an effective option without intestinal rerouting.
Weight loss is usually strong, and most individuals see improvements in conditions like high blood pressure or prediabetes within the first year. Some people lose a bit less weight than they might with bypass or duodenal switch procedures, but the results are still significant.
One thing we always discuss as Registered Dietitians is reflux. Some people who already struggle with GERD notice that symptoms stay the same or worsen after a sleeve. For others, it’s not an issue at all. The key is making sure your surgeon evaluates your symptoms, lifestyle, and long-term goals so the sleeve truly fits your needs.

Roux-en-Y Gastric Bypass (RYGB)
Gastric bypass creates a small upper stomach pouch and reroutes part of the small intestine. This approach limits portion size and reduces calorie absorption, creating a powerful combination for weight and metabolic change.
Many people see improvements in type 2 diabetes even before significant weight loss occurs because the procedure influences hormones involved in blood sugar control. Weight loss tends to be strong and steady, which is one reason bypass remains one of the most widely performed surgeries worldwide.
At the same time, there are important considerations. Nutrient deficiencies can occur more easily because food bypasses key absorption sites, so lifelong supplements and regular lab monitoring are essential.
Some people experience dumping syndrome, a rapid shift of food into the intestine that can cause nausea or a racing heartbeat after high-sugar meals. It’s manageable but worth understanding in advance.
For individuals struggling with reflux, bypass often provides relief. For those wanting a balance of strong metabolic impact and long-term durability, this procedure is a common choice.
Duodenal Switch & SADI-S/SIPS
The duodenal switch and its simplified versions, like SADI-S or SIPS, combine a sleeve gastrectomy with a more extensive bypass of the intestines. This mix offers both restriction and significant metabolic effects.
These procedures tend to create substantial and long-lasting weight loss, especially for individuals with very high BMI or advanced metabolic disease. Many people with severe type 2 diabetes see dramatic improvements in blood sugar control.
The SADI-S version uses a single connection rather than two, which can reduce some surgical risks while keeping the core benefits.
While the results are impressive, the nutritional demands are higher than with other surgeries. People need consistent follow-up, regular blood work, and a strong supplement routine to prevent deficiencies. Protein intake becomes especially important because the body absorbs less than it used to.
From our experience, people who choose these surgeries usually appreciate the potential for robust results but also understand the commitment required to maintain their health. It’s a powerful option when chosen thoughtfully with a skilled surgical team.

Adjustable Gastric Band
The adjustable gastric band is placed around the top portion of the stomach to create a small pouch that controls how much food enters the stomach at once. It’s less invasive than other surgeries and has an adjustable component, which originally made it appealing.
Over time, though, many centres have moved away from this option because long-term outcomes haven’t matched those of sleeve or bypass. Issues like band slippage, erosion, or chronic discomfort became more common than hoped, and many people eventually needed the band removed or replaced with a different surgery.
Weight loss tends to be slower and less predictable compared with other procedures. Some individuals do well with it, especially if they’re highly motivated and have strong follow-up support, but it’s now used far less frequently in high-volume bariatric programs.
When people come to us asking about the band, we help them look closely at long-term expectations, maintenance requirements, and the potential need for future surgery. That context helps them choose a path that truly supports their goals.
Endoscopic & “Non-Surgical” Procedures
Minimally invasive and non-surgical options can be helpful for people who want meaningful support without committing to a major operation. These procedures work well for certain BMI ranges, for individuals with specific health needs, or for those who want a stepping-stone approach.
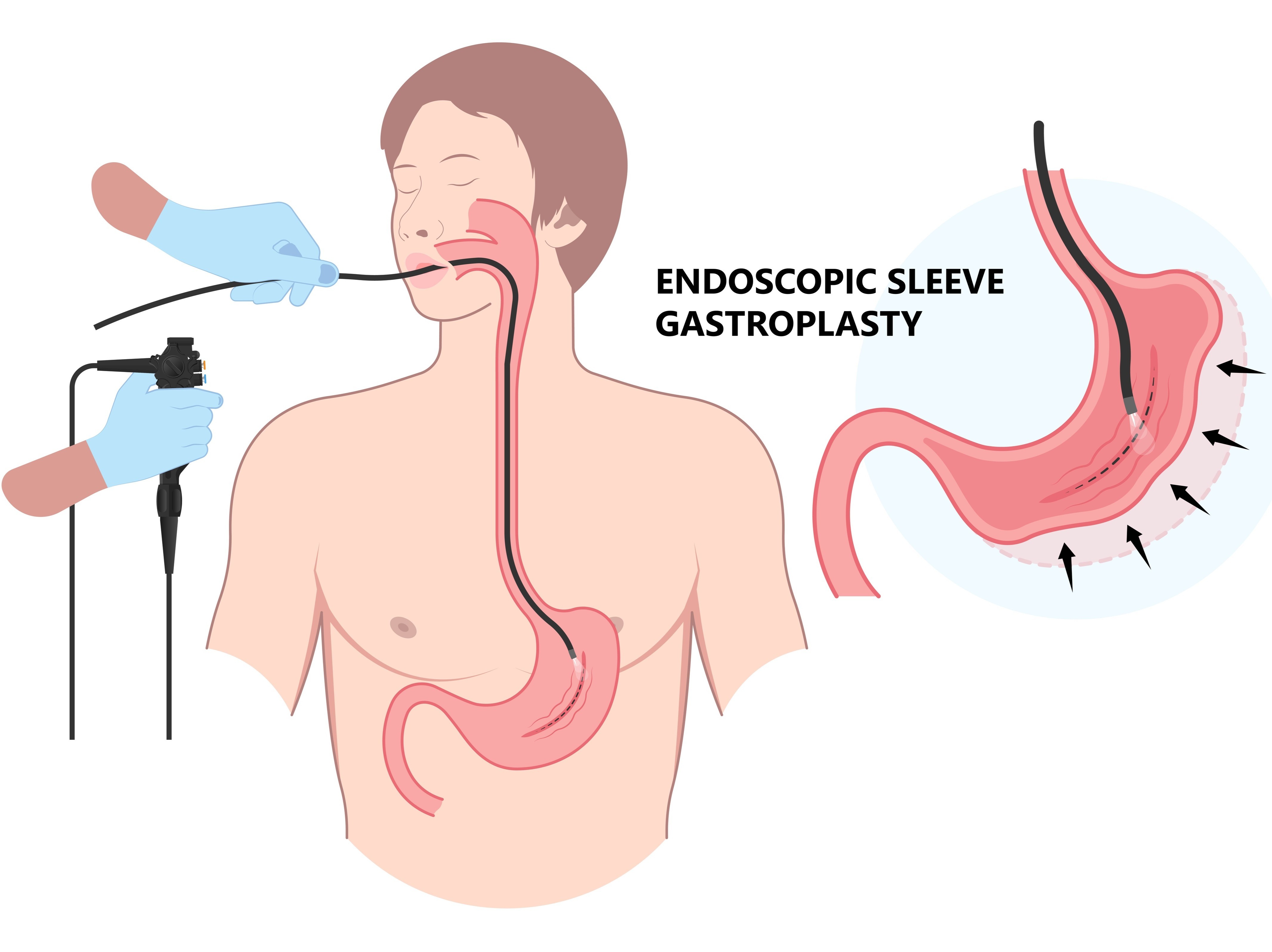
Endoscopic Sleeve Gastroplasty (ESG)
Endoscopic sleeve gastroplasty uses a flexible scope inserted through the mouth to place sutures inside the stomach. Those sutures reduce stomach volume, so you feel full sooner and eat smaller portions naturally. There are no external incisions, which means quicker recovery and fewer surgical risks.
People often return to normal activities faster than they would after traditional surgery. ESG tends to work best for individuals with lower BMI ranges or those who want a less intensive option.
Weight loss can be meaningful, especially when paired with consistent nutrition and behavioural support. It’s also helpful for people who aren’t ready for a permanent anatomical change but still want structured assistance with appetite control. Since the stomach remains intact, long-term nutritional risks are lower, though ongoing lifestyle work is still essential.
Intragastric Balloon
The intragastric balloon is placed through the mouth and positioned in the stomach, then filled with saline to help create a sense of fullness. It’s temporary and usually stays in place for six months before removal. Many people appreciate that it offers a defined timeframe with structured support.
It can help break through plateaus, jump-start weight loss, or serve as a bridge to future surgery if someone needs to reduce surgical risk. Weight loss results vary, but people often see steady progress while the balloon is in place.
Once it’s removed, continued nutrition guidance is key to maintaining momentum. This option can be especially appealing for those who want a non-surgical tool with a shorter commitment and a lower risk profile. When used thoughtfully within a structured program, it can open the door to better habits and improved confidence.
How Much Weight Can You Expect to Lose from Surgery?
Weight loss varies by procedure, starting weight, and how closely someone follows nutrition and lifestyle recommendations. Most people see the fastest changes in the first six months, then continued steady progress through the first one to two years. The data below gives you a realistic picture of what different surgeries typically produce, so you can compare them side by side:
Gastric Bypass (RYGB): About 60 to 70% excess weight loss within 12 to 18 months.
Sleeve Gastrectomy (VSG): About 50 to 60% excess weight loss in the first 12 to 18 months.
Duodenal Switch (including SADI-S/SIPS): Often 70 to 80% excess weight loss with strong long-term durability.
Adjustable Gastric Band: Typically 35 to 45% excess weight loss, with slower and more variable results.
Long-term outcomes improve most when protein, supplements, movement, and regular follow-up stay consistent.

Are You Eligible for Weight Loss Surgery?
Eligibility is an important part of the decision-making process, since surgery is a medical treatment with specific criteria. Knowing what surgeons and insurers look for helps you prepare and sets clear expectations from the very beginning.
Adult Criteria & What Insurers Look For
Adults are usually evaluated using BMI ranges and the presence of significant health conditions. Most people qualify with a BMI of 40 or higher, or a BMI between 35 and 39.9 paired with issues like type 2 diabetes, severe sleep apnea, or high blood pressure.
Some insurers may approve individuals with a BMI of 30 to 34.9 if their medical conditions are serious and well-documented. Insurance companies often require proof of previous supervised weight-loss efforts, which might include visits with a Registered Dietitian or participation in structured programs. Many plans also ask for a psychological evaluation to confirm readiness for the lifestyle changes ahead.
Nicotine use is another major factor, since smoking increases surgical risk, and most insurers require that someone be nicotine-free before approval. Documentation is everything, so gathering medical records, lab results, and comorbidity notes early makes the process smoother.
Teen & Young Adult Eligibility
Teens and young adults follow similar criteria, but there’s more emphasis on safety, developmental readiness, and strong long-term support. Most programs consider surgery for adolescents with class II or class III obesity, especially if conditions like type 2 diabetes, fatty liver disease, sleep apnea, or hypertension are present.
Comprehensive bariatric centers tailor the evaluation to younger patients, making sure growth, emotional development, and social factors are considered. These teams often include surgeons, pediatricians, psychologists, exercise specialists, and Registered Dietitians who understand the unique needs of this age group.
The goal is to confirm that the teen can follow post-surgery nutrition guidelines, attend regular follow-ups, and manage supplements independently or with family support. Families also play a major role, since consistent structure at home increases long-term success. When all of these pieces align, surgery can be a safe and effective option for reducing health risks early in life.

Pre-Op Work-up & Mandatory Programs
The pre-operative phase helps ensure that surgery is safe and that someone is fully prepared for the lifestyle changes ahead. It typically starts with a detailed nutrition assessment where a Registered Dietitian reviews current eating patterns, medical history, and habits that might affect recovery.
Lab work, cardiac evaluations, and sleep studies may also be ordered, depending on a person’s health. Psychological assessments help identify emotional readiness, coping skills, and potential areas where extra support might be helpful.
Many programs also require short pre-surgery education modules or classes to explain what eating will look like after surgery, how to take supplements correctly, and how to progress through the staged diet. Some insurers mandate a supervised weight-management program lasting several weeks or months.
While this can feel like a hurdle, it often helps people build momentum and feel more confident before surgery. This preparation phase strengthens long-term outcomes and sets the foundation for lasting success.
Costs, Financing & Insurance Coverage for Weight Loss Surgery
Money questions come up quickly when someone starts exploring surgery, and for good reason. Prices vary a lot between procedures and insurance plans, so getting a clear picture of what things typically cost and how coverage works can make the whole process feel less confusing.
Typical Price Ranges
Surgery costs vary a lot depending on location, hospital fees, surgeon experience, and insurance contracts. Seeing real numbers helps you compare options and budget realistically, especially if part of the cost may fall on you:
Sleeve Gastrectomy (VSG): Typically $15,000 to $38,000 in the United States.
Roux-en-Y Gastric Bypass (RYGB): Usually $15,000 to $25,000, often higher due to longer operating time.
Duodenal Switch / SADI-S: Commonly $25,000 to $40,000, sometimes more depending on surgical complexity.
Adjustable Gastric Band: Generally $8,000 to $27,000, though long-term maintenance costs can increase total spending.
Endoscopic Sleeve Gastroplasty (ESG): Often $8,000 to $15,000, typically self-pay.
Intragastric Balloon: Typically $6,000 to $10,000 for placement and removal.
These ranges may shift depending on whether a provider is in-network, which services are bundled, and how follow-up care is billed.
Will Insurance Cover It?
Insurance coverage depends on meeting the plan’s medical necessity requirements and completing all required documentation. Most insurers cover sleeve, bypass, and duodenal switch when someone meets BMI criteria and has documented comorbidities, but each policy has its own rules.
Prior authorisation is common, which means your surgical team must submit notes, records, and evaluations before you’re approved. Some plans require a supervised weight-management program, usually lasting three to six months, before they’ll approve the procedure. Others may have specific exclusions for certain surgeries or for individuals below a particular BMI.
Nicotine use is a frequent barrier because many insurers require people to be nicotine-free for several weeks before surgery. It helps to call your insurance provider early and ask detailed questions so you know exactly what paperwork and timing to expect. Preparation makes the process far less stressful.
Financing Options
If insurance doesn’t cover surgery or only covers part of the cost, there are several ways to manage payments without feeling overwhelmed. Many people use health savings accounts or flexible spending accounts, which allow pre-tax dollars to go toward medical expenses. Some surgical centres offer payment plans with predictable monthly payments, which can help spread out costs in a manageable way.
Medical loans are another option, though it’s important to review interest rates and repayment terms carefully. A smaller number of people qualify for grants or financial-assistance programs designed for individuals seeking bariatric surgery.
These options can be helpful when finances are tight or when insurance excludes the procedure entirely. It’s also worth asking your surgical team which financing resources they recommend, since they often know which lenders or programs are reliable. The goal is to build a plan that supports your health without creating unnecessary financial strain.

How to Choose the Right Procedure for You
Choosing a surgery is a personal decision, and it helps to look at your health, your habits, and what you want long-term. These factors give you a clearer sense of which procedure fits your needs rather than relying only on popularity or general recommendations.
1. Your Medical Conditions
Your current health plays a major role in selecting the most effective option. People with severe type 2 diabetes or higher BMI ranges often benefit more from stronger metabolic procedures such as gastric bypass, duodenal switch, or SADI-S, since these surgeries create meaningful changes in hormone regulation and blood sugar control.
If you’re dealing with conditions like fatty liver disease, high blood pressure, or severe sleep apnea, your surgical team may lean toward a more powerful approach because the metabolic improvements can be substantial.
Bariatric surgery can also help with certain thyroid issues, such as losing weight with hypothyroidism. If you're dealing with this or are struggling to lose weight with Hashimoto’s, your surgical team can assess the best treatment for you.
On the other hand, if your primary concerns are related to moderate weight challenges or early-stage health issues, a sleeve may provide enough support without the added complexity.
As Registered Dietitians, we also look at how your health conditions affect nutrition needs. For example, iron-deficiency anemia may influence the choice, since bypass procedures can impact nutrient absorption. Matching your surgery to your medical picture helps ensure the benefits align with your needs.

2. Reflux History
Your digestive symptoms influence your surgical options more than many people expect. Chronic GERD is one of the strongest predictors of which direction a surgeon may recommend.
If you regularly experience acid reflux, heartburn, or regurgitation, gastric bypass is often the safer and more comfortable long-term choice because it reduces pressure on the stomach and generally improves reflux.
Sleeve gastrectomy can sometimes make symptoms worse, especially for people who already struggle with daily discomfort. That doesn’t mean the sleeve is off the table entirely, but it does mean your team will want to evaluate tests like endoscopy findings or pH studies. Even mild reflux matters because post-surgery reflux can affect your quality of life, sleep, and food tolerance.
Thinking about how your body feels day to day helps you choose the procedure that supports long-term comfort rather than creating new challenges.
3. Your Lifestyle and Preferences
Your daily habits and personal style play a bigger role than many people expect. Some people prefer a procedure with fewer anatomical changes, shorter hospital stays, or simpler long-term maintenance. Others want the most powerful metabolic effects and are comfortable with a more complex surgery.
If your lifestyle involves frequent travel, unpredictable schedules, or limited time for appointments, you may gravitate toward a sleeve or an endoscopic option because the follow-up can be a bit easier to manage. If you enjoy structure and don’t mind regular check-ins, bypass or duodenal switch may feel like a manageable fit.
Your comfort level with recovery time matters, too. Some procedures require more gradual diet progression and longer adjustment periods. Thinking through how you naturally operate day to day helps you choose a surgery that supports your routine rather than works against it.

4. Nutritional Follow-Through
Every surgery requires ongoing nutrition support, but some require more intensive supplementation and lab monitoring. Gastric bypass, duodenal switch, and SADI-S all involve some degree of malabsorption, which means your body absorbs fewer nutrients. That’s effective for weight loss, but it also means you’ll need daily vitamins, protein-focused eating, and scheduled lab work.
If you know regular follow-up feels achievable, these procedures can be great options. If consistent supplement use or lab monitoring feels challenging, a sleeve or an endoscopic procedure may be a better fit because the nutritional demands are lighter.
As Registered Dietitians, we see how follow-through affects long-term success. People who choose procedures that match their ability to maintain nutrition routines tend to feel happier with their results and avoid complications. Being realistic about your comfort with structure helps you choose a surgery that supports your health without creating unnecessary stress.
5. Long-Term Goals
Your specific goals help shape the right choice, especially when it comes to health improvements. If you want stronger chances of diabetes remission, metabolic normalization, or lowering multiple medications, gastric bypass or duodenal switch procedures may align more closely with your priorities.
If your goals centre around reducing joint pain, improving mobility, and feeling more comfortable day to day, sleeve gastrectomy may provide the level of change you’re looking for. Some people prioritise keeping the digestive pathway as intact as possible, while others focus more on maximum weight loss potential.
Goals like pregnancy planning, athletic performance, and future medical needs can also influence the decision. Your long-term vision matters because it shapes the type of progress you want to see over years, not just months. The right surgery should support both your health and the kind of life you want to build.

6. Your Relationship With Food and Eating Patterns
Your eating habits and emotional patterns around food are important pieces of the puzzle. Some procedures, like gastric bypass, tend to reduce cravings for sweets and high-sugar foods because they influence gut hormones and can trigger unpleasant symptoms like dumping syndrome when sugary foods are eaten too quickly.
The sleeve may work well for people who struggle more with portion sizes than cravings. If emotional eating, binge eating, or nighttime grazing are concerns, it helps to consider how each procedure will interact with those tendencies.
Working with a Registered Dietitian or therapist can highlight which patterns feel most challenging for you. Surgery doesn’t remove these habits entirely, but certain procedures can make them easier to manage. Matching the surgery to your relationship with food helps set you up for sustainable change rather than short-term results.
7. Recovery Time and Daily Responsibilities
Your responsibilities outside the hospital matter, especially when considering how much time you’ll need to recover. Traditional surgeries like bypass or sleeve often require a few weeks of reduced activity, while endoscopic approaches may allow you to return to normal routines much sooner. If you have caregiving duties, limited time off work, or physical job demands, these details can influence your choice.
Some people feel more comfortable with a faster recovery, even if the weight loss is less dramatic. Others have the flexibility to focus on a longer healing period and choose a procedure with more substantial long-term impact. Thinking about your responsibilities helps you choose an option that fits your life without unnecessary strain. Recovery should feel manageable, not disruptive.

Benefits of Weight Loss Surgery
There are many reasons people consider weight loss surgery, and most of them come down to wanting a healthier, more comfortable life. These benefits show up in different ways, and each one can make daily routines feel easier and more enjoyable.
1. Significant Long-Term Weight Loss
Long-term weight loss is one of the biggest reasons people choose surgery, because it creates changes that are difficult to achieve through lifestyle alone. Most individuals lose the majority of their excess weight within the first one to two years, and many maintain those results long term when supported by good nutrition and consistent follow-up.
That kind of progress can lead to easier movement, more stamina, and greater confidence during everyday activities. Things like climbing stairs, going for walks, or fitting comfortably in chairs often feel noticeably better within months. People also tend to see improvements in clothing fit and mobility, which adds a sense of momentum.
We often see how these changes lift people’s mood and weight loss motivation. Weight loss surgery gives you a tool that supports sustained progress, making health improvements feel more achievable and less exhausting.
2. Improvement of Obesity-Related Conditions
Weight loss surgery often improves or resolves conditions that have been difficult to manage with medication alone. Many people see better blood sugar control, reduced A1C levels, and a meaningful drop in diabetes medication needs. Sleep apnea often improves as the airway becomes less compressed, which supports better rest and daytime energy.
Blood pressure, cholesterol levels, and inflammation can also decrease as the body adapts to a lighter weight and improved metabolism. Joint pain tends to ease as pressure on knees and hips decreases, making movement less uncomfortable.
These physical changes help people return to activities they may have avoided for years. In our experience, the health improvements can be just as meaningful as the weight changes. They support long-term health in ways that open the door to a fuller and more active life.

3. Increased Longevity and Better Quality of Life
Many people choose surgery because they want not only more years, but better years. Research consistently shows that weight loss surgery reduces the risk of early death linked to obesity-related conditions. Better mobility, more stable energy, and easier breathing all contribute to feeling more capable and more engaged in daily life.
Clients often report improvements in mental well-being, including reduced anxiety around health concerns and increased confidence when moving through the world. Everyday tasks like shopping, traveling, or caring for family members become more manageable.
Over time, these changes combine to create a stronger sense of independence and control. When someone feels better physically, it’s easier to build a life that feels enjoyable and meaningful.
4. Positive Metabolic Changes
The metabolic effects of surgery are powerful and often show up quickly. Procedures like gastric bypass and sleeve gastrectomy influence hormones that regulate hunger, fullness, and blood sugar.
These shifts help reduce cravings, support more stable energy, and make it easier to follow a balanced eating pattern. Many people notice that foods they used to overeat suddenly feel less appealing, which creates a helpful mental reset.
Blood sugar control tends to improve almost immediately, which can be especially impactful for people managing type 2 diabetes. The body also becomes more responsive to insulin, making glucose regulation smoother.
These changes support long-term weight maintenance and better metabolic health. With consistent nutrition support, people learn how to use these advantages to build habits that last. It’s an internal shift that supports the external progress you see on the scale.

5. Improved Emotional and Social Well-Being
Emotional well-being often changes in ways that feel just as meaningful as the physical results. Many people experience a boost in confidence as they feel more comfortable in their bodies and more capable in their daily routines. Social interactions can feel easier when activities like dining out, traveling, or attending events no longer trigger stress or physical discomfort.
Improved mobility also opens the door to hobbies or movements that weren’t accessible before, which can reduce feelings of isolation.
For some, the biggest changes happen quietly, like feeling less self-conscious walking into a gym or trying on new clothing. Many people also describe feeling more hopeful about their health and future. With the right support system, these emotional improvements reinforce long-term success and help create a more fulfilling lifestyle.
Risks and Side Effects of Weight Loss Surgery
Every medical procedure comes with risks, and weight loss surgery is no different. Knowing what to expect helps you make informed decisions and prepares you for the long-term commitments that support the best outcomes.
1. Surgical Complications
Surgical complications can happen with any operation, and bariatric procedures are no exception. Most people do very well, but there is still a small risk of bleeding, infection, or reactions to anesthesia.
Some individuals may experience leaks at surgical connection points, which require immediate medical attention. Blood clots are another concern, especially for people with limited mobility, which is why early walking and preventive medication are part of recovery.
While the risk of life-threatening complications is low, it’s important to talk openly with your surgeon about your medical history so they can plan safely. Strong pre-operative care, good surgical technique, and careful follow-up all help reduce risks. Understanding these possibilities helps you approach the process with confidence rather than fear.

2. Nutrient Deficiencies
Nutrient deficiencies are a long-term consideration, especially for procedures that involve intestinal rerouting, such as gastric bypass or duodenal switch. These surgeries can affect how well your body absorbs iron, vitamin B12, calcium, vitamin D, and sometimes protein.
Daily supplements aren’t optional. They’re a core part of protecting your health after surgery. Regular blood work helps catch deficiencies early so they can be corrected before symptoms like fatigue, hair loss, or anemia become more significant.
From our experience as Registered Dietitians, people who stay consistent with supplements and follow-up labs are far less likely to run into problems. It helps to choose a procedure that matches your ability to manage long-term nutrition routines. With the right support, deficiencies can be prevented, but it’s important to take them seriously.
3. Weight Regain
Weight regain can happen after any bariatric procedure. Most people lose a significant amount in the first one to two years, but long-term results depend heavily on habits, follow-up, and lifestyle support.
Regain may occur if someone returns to larger portions, frequent grazing, or high-calorie beverages. For some individuals, changes in anatomy over time, such as pouch stretching or hormonal shifts, can also play a role.
Regular visits with a Registered Dietitian, structured meal patterns, and behavioural support help maintain weight loss and reduce the risk of regain. Many people find that adding movement, stress management, and consistent protein intake keeps things more stable.
If a regain happens, it’s not a failure. It’s a signal to reconnect with your team and make adjustments before small changes become bigger challenges.

4. Procedure-Specific Concerns
Each type of surgery comes with unique considerations. Sleeve gastrectomy can worsen reflux for some people, especially if they already struggle with heartburn. Gastric bypass may trigger dumping syndrome, which causes nausea, lightheadedness, or rapid heartbeat after eating sugary foods.
Adjustable gastric bands can slip, erode, or cause long-term discomfort, which is why they’re used less frequently today. Duodenal switch procedures carry a higher risk of malabsorption, which can cause gastrointestinal symptoms if supplements and protein intake aren’t maintained.
These risks don’t mean the procedures are unsafe. They simply highlight the importance of choosing a surgery that matches your health needs, lifestyle, and ability to maintain follow-through. Talking through these details with your surgical and nutrition team helps you choose a procedure with fewer unexpected challenges.
5. Emotional and Mental Health Shifts
Emotional changes are an often-overlooked part of the process. Many people feel proud, excited, and relieved as the weight comes off, but others experience stress, anxiety, or unexpected emotions around their rapid weight loss.
Eating patterns may shift dramatically, which can bring old habits or coping strategies to the surface. Social situations may feel different, too. For example, dining with friends may require new boundaries or planning.
Body image may take time to catch up to physical changes, and that adjustment can feel confusing or overwhelming.
Support from mental health professionals and Registered Dietitians makes this transition easier. These emotional shifts don’t mean surgery was the wrong choice. They simply confirm that weight loss affects more than the physical body, and support systems make the process smoother and healthier.
Because weight loss surgery carries meaningful risks and long-term commitments, we recommend exploring nutrition-focused strategies first. A Registered Weight Loss Dietitian can help you create a personalized 7-day meal plan tailored to your goals, medical history, and lifestyle, giving you a safer starting point before considering surgery.

How to Prepare for Weight Loss Surgery
Preparation plays a huge role in how smoothly surgery and recovery go. Each step helps you build confidence, strengthen your habits, and understand what your body needs both before and after the procedure.
Step 1: Educate Yourself
Learning what to expect sets the foundation for a smoother experience. People who understand their procedure, recovery timeline, and long-term commitments tend to feel more confident and supported.
Education usually begins with meetings led by your bariatric team, including a surgeon, a Registered Dietitian, and often a psychologist. You’ll walk through how the surgery works, what the staged diet looks like, and which behaviours make the biggest difference during recovery.
Many programs offer classes or online modules that explain portion sizes, hydration habits, and supplement routines. These resources help you understand how your body will feel right after surgery and how to manage early challenges like fatigue or changes in appetite.
Ask questions, take notes, and talk openly about any concerns. Clear expectations reduce stress and make the transition into post-op life more manageable.
Step 2: Begin Nutrition Changes
Nutrition preparation is one of the most important steps, because your eating habits directly influence your recovery and long-term results. You’ll meet with a Registered Dietitian who teaches you how to structure meals, prioritise protein, and practice mindful eating.
Many people start by reducing sugary drinks, planning regular meals, and getting comfortable with smaller portions. Hydration becomes a major focus, since you’ll need to sip water consistently after surgery.
Pre-op nutrition also helps shrink the liver, which gives the surgeon better access during the procedure. Some programs recommend a short pre-operative diet to support this process.
You’ll also go over the vitamin and mineral supplements you’ll need after surgery, so there are no surprises later. These early changes help you ease into the post-op lifestyle instead of feeling overwhelmed.

Step 3: Complete All Medical Clearances
The medical clearance process ensures that surgery is safe for you and that your team understands your full health picture. You may complete blood work, an EKG, a sleep study, chest imaging, or additional testing based on your medical history.
Psychological evaluations help confirm emotional readiness and identify areas where extra support will be useful.
If you have conditions like diabetes, asthma, or high blood pressure, your provider may recommend adjustments to your medications before surgery.
People who use nicotine are usually required to stop several weeks beforehand, because nicotine increases the risk of complications.
Sometimes specialists, such as cardiologists or pulmonologists, are involved to confirm that your body can handle anesthesia and recovery. These steps make surgery safer and help your team customise your care.
Step 4: Plan Your Lifestyle and Home Setup
Your daily routine shapes your recovery, so planning ahead helps things run smoothly. Start by arranging support at home, whether that means help with childcare, pets, or meals during the first few days.
Preparing your kitchen with broth, protein shakes, and hydration supplies saves stress later. Many people set up a comfortable recovery area with pillows, blankets, and easy access to water.
You’ll also plan your time off work and review any activity restrictions with your surgeon. Scheduling follow-up appointments, nutrition check-ins, and lab work ahead of time keeps you on track.
These details might seem small, but they make the early recovery period much easier. When your environment supports your goals, it’s simpler to stick to the plan.
Step 5: Build a Gentle Movement Routine
Gentle physical activity before surgery can make recovery smoother and improve how your body handles the procedure. You don’t need intense workouts. Even short daily walks or light strength exercises can help build stamina and support healthy circulation.
If joint pain limits your movement, low-impact activities like swimming or stationary biking can be great alternatives.
Your care team may recommend simple breathing exercises to strengthen your lungs before anesthesia.
These habits also help you transition into the post-op movement routine, since walking is encouraged within hours after surgery. Think of this step as preparing your body to heal more comfortably.
When you enter surgery feeling conditioned and supported, your recovery often feels less overwhelming. Small, consistent movement builds confidence and sets you up for long-term success.
Weight Loss Surgery Recovery Best Practices
Recovery is a gradual process, and the habits you build in these early weeks shape your long-term results. These tips help you heal comfortably and avoid the most common post-surgery setbacks:
1. Follow the Staged Diet Carefully
Your digestive system needs time to heal, and the staged diet protects the surgical site while helping you ease into new eating patterns. You’ll start with clear liquids, then move to full liquids, purees, soft foods, and eventually regular textures. This sequence helps prevent nausea, vomiting, or discomfort during the early healing phase.
Eating slowly makes a real difference, too, because even soft foods can feel surprisingly filling in a smaller stomach.
Your Registered Dietitian will guide you on portion sizes and meal timing so you feel supported every step of the way. It’s normal to feel unsure at first, but sticking to the plan gives your body the best chance to heal. Think of it as creating a strong foundation for all the progress that comes next.

2. Prioritise Protein and Hydration
Protein and hydration are essential for healing after surgery. Protein supports tissue repair, maintains muscle mass, and keeps energy levels steadier throughout the day. Many people aim for small, frequent meals with protein-rich foods like yogurt, cottage cheese, or blended soups during early recovery.
Hydration is just as important. You’ll need to sip water consistently, since drinking large amounts at once can cause discomfort. Dehydration is one of the most common reasons people return to the hospital after surgery, so keeping fluids nearby makes a big difference.
Electrolyte drinks without added sugar can help on days when water feels difficult. These habits may feel new, but with practice, they become second nature and help you feel your best.
3. Stay Active Safely
Gentle movement supports healing and reduces the risk of complications such as blood clots. Most people begin walking the same day as surgery, even if it’s just short, slow laps around the hospital room. These small steps help stimulate circulation and reduce stiffness.
As you return home, brief walks throughout the day are more helpful than one long walk. You don’t need structured exercise yet. Just simple movement that keeps your body engaged.
Avoid lifting heavy objects or pushing yourself too hard until your surgeon clears you. Pay attention to how your body feels, and increase activity gradually. This early movement sets the stage for a smoother transition into regular exercise later on.

4. Watch for Concerning Symptoms
Your body sends clear signals when something isn’t right, and it’s important to take those signs seriously during recovery. Persistent vomiting, severe abdominal pain, dehydration, rapid heartbeat, or difficulty breathing all require prompt medical attention. These symptoms may indicate complications such as strictures, leaks, or nutritional imbalances.
Keep your surgical team’s contact information somewhere visible so you never hesitate to reach out. Even if you’re unsure whether something is normal, it’s always better to ask. Early intervention prevents small issues from becoming bigger problems.
Tracking your symptoms, fluid intake, and bowel habits during the first few weeks can help you catch concerns early. Your care team is there to support you, so staying connected helps you feel safe and informed.
5. Use Psychological and Behavioral Support
Surgery changes how your stomach functions, but emotional patterns and food habits often take longer to adjust. Many people notice shifts in mood, cravings, or coping strategies during recovery. This is completely normal.
Support from a psychologist, therapist, or Registered Dietitian can help you navigate these changes with confidence. You may explore new ways to manage stress, boredom, or social situations.
Some people find it helpful to journal or track emotions alongside eating habits. Others join support groups to connect with people who understand the process.
These tools help you build a healthier relationship with food and set the groundwork for long-lasting success. Recovery is about more than healing physically. It’s about building sustainable habits that support your goals.

6. Keep Follow-Up Appointments Consistent
Regular follow-ups help your team monitor your progress and catch concerns early. These visits allow your surgeon and Registered Dietitian to assess healing, nutrition status, lab values, and weight trends.
Even if you feel great, these appointments are essential. They’re opportunities to fine-tune your supplement routine, adjust protein goals, or troubleshoot challenges like constipation or low energy.
Many people find that consistent check-ins keep them motivated and accountable. Virtual appointments or support groups can help if in-person visits are hard to schedule. Staying connected with your team gives you the guidance you need as your body adapts.
7. Prepare for Changing Food Tolerances
Your taste preferences and food tolerances may shift during recovery, and being flexible helps you adapt more easily. Foods you enjoyed before surgery may feel too heavy or too sweet, especially during the first couple of months. Many people discover new favourites, such as lighter proteins or softer textures.
Keeping an open mind makes the process smoother. If something bothers your stomach, wait a week and try again. Your Registered Dietitian will help you identify which foods typically work well and which ones to avoid temporarily. These changes are normal and often temporary.
Over time, most people regain tolerance for a wide variety of foods, as long as they reintroduce them gradually and listen to their body’s cues.

Special Considerations for Weight Loss Surgery
Some health situations call for a closer look before choosing a procedure, because certain factors can change what’s safest or most effective. These considerations help shape a plan that fits your anatomy, your medical history, and your long-term goals.
Higher-BMI or Severe Metabolic Disease
People with higher BMI ranges or advanced metabolic conditions often require a more powerful surgical approach to see meaningful improvements. Procedures like the duodenal switch or SADI offer strong and durable weight loss because they combine restriction with significant changes in how the body absorbs nutrients.
These operations also have a notable impact on hormone regulation, which can dramatically improve conditions like type 2 diabetes or severe insulin resistance. For individuals with BMIs above 50, these benefits often outweigh the added complexity of the surgery.
At the same time, these procedures require consistent long-term follow-up. Daily supplements, high-protein eating, and frequent lab checks are essential to protect against deficiencies.
People who choose these surgeries often value their strong metabolic effect and are ready to commit to the nutritional structure required. With the right support team, these procedures can be life-changing for those facing serious health risks tied to excess weight.

Reflux or Prior Abdominal Surgery
Reflux history has a big influence on which procedure will feel most comfortable long-term. People with moderate to severe GERD often do better with gastric bypass because it reduces acid exposure and helps limit reflux symptoms.
Sleeve gastrectomy, on the other hand, may worsen heartburn for some individuals, especially when symptoms are already present before surgery.
Surgeons also consider previous abdominal operations, since scar tissue or altered anatomy can affect how safely a particular procedure can be performed. Someone who has had multiple abdominal surgeries might be steered toward a sleeve if bypass poses a higher technical risk, or vice versa, depending on the specific operative history.
These considerations help your team recommend an option that works with your anatomy instead of complicating it. Talking honestly about your symptoms and history ensures the final choice supports both comfort and long-term success.
When Revision and Conversion Surgeries Might Be Necessary
Revision or conversion surgeries are sometimes needed when the initial procedure no longer meets a person’s health goals or when complications appear over time.
Some people experience limited weight loss after their first surgery or begin regaining weight due to changes in appetite patterns, anatomy, or hormone responses. In these cases, converting a sleeve to a gastric bypass or adding a malabsorptive component may provide the additional support needed.
Other revisions are done to address medical issues. For example, severe reflux after a sleeve may lead to conversion to bypass, or long-term complications from an adjustable gastric band may require removal.
Revision surgeries are more complex than primary procedures, which is why ongoing follow-up with your bariatric team is so important. Early detection of concerns makes interventions smoother and safer. Revisions offer a path forward for people who need renewed support in their weight management journey.

Panniculectomy vs Abdominoplasty
Loose skin after weight loss can be very common, especially after losing a large amount of weight over a relatively short time.
Many people start thinking about skin removal once their weight has been stable for at least 12 to 18 months, since that’s when the body is more likely to have settled. It’s not medically required for everyone, but it can make a real difference in comfort, confidence, and day-to-day function.
Some people struggle with recurring rashes, skin breakdown, chafing, or difficulty keeping skin folds clean and dry. Others feel held back in exercise or movement because the extra skin pulls or feels heavy.
There’s also a very real emotional side, where someone may feel that their outside doesn’t match the hard work they’ve put in. Talking with a plastic or reconstructive surgeon helps you explore realistic outcomes, timing, and whether medical or cosmetic goals are your priority.
Panniculectomy vs Abdominoplasty
A panniculectomy and an abdominoplasty both focus on the abdomen, but they’re designed for different needs.
A panniculectomy targets the hanging “apron” of skin low on the belly that can trap moisture, cause recurrent rashes, and make walking or exercise uncomfortable. Because it addresses functional problems like infections or skin breakdown, it’s sometimes covered by insurance when there’s solid documentation from your healthcare team.
An abdominoplasty, or tummy tuck, goes a step further by tightening the abdominal muscles, repositioning the skin, and reshaping the waistline. It’s usually considered cosmetic, so most insurance plans don’t cover it.
Both procedures come with scars, downtime, and specific recovery instructions, so planning time off and support at home matters. Surgeons generally prefer that your weight has been stable for 12 to 18 months before either option.

Feature | Panniculectomy | Abdominoplasty (Tummy Tuck) |
Primary Purpose | Removes overhanging skin for medical relief | Improves contour and tightens abdominal muscles |
Insurance Coverage | Often covered if medical issues are documented | Usually not covered; considered cosmetic |
Muscle Repair | No | Yes |
Aesthetic Outcome | Functional improvement | More sculpted appearance |
Best For | Rashes, irritation, hygiene challenges | Cosmetic reshaping after weight loss |
Timing | After 12–18 months of weight stability | After 12–18 months of weight stability |
Non-Surgical Paths for Weight Loss and When to Combine Treatments
Non-surgical strategies can be incredibly helpful, whether you’re preparing for surgery, trying to avoid surgery, or maintaining results afterward. These options give you more flexibility, and many people find they work best when combined with structured nutrition and ongoing support.
GLP-1/GIP Medications
GLP-1 and GIP medications have become a major part of modern weight management because they help regulate appetite, reduce cravings, and support healthier blood sugar levels.
These medications slow gastric emptying and make it easier to feel satisfied with smaller portions, which can be especially helpful for people who struggle with constant hunger. They’re often used before surgery to reduce surgical risk, or after surgery to help maintain long-term progress.
People also turn to these medications when they want a non-surgical option or when medical conditions make surgery less ideal.
Side effects like nausea or constipation can happen, so guidance from a Registered GLP-1 Dietitian helps you adjust eating patterns and manage symptoms. These medications work best when paired with thoughtful nutrition, steady routines, and regular follow-up. They’re a flexible tool that can support different stages of a weight-loss journey.

Lifestyle Changes
Lifestyle changes remain the foundation of sustainable weight management, whether someone chooses surgery, medications, or a non-surgical path. Consistent nutrition habits, regular movement, and behavioural support help you build a routine that feels steady instead of overwhelming.
Many people start with simple changes like adding protein to each meal, drinking more water, or taking a daily walk. These small actions create real momentum. Stress management also matters because high stress can increase cravings and disrupt sleep, which affects appetite regulation.
Working with a Registered Health Dietitian helps you personalise your plan and stay accountable in a way that feels supported rather than rigid. You might explore meal planning, mindful eating, or strategies that help reduce nighttime snacking.
Over time, these habits build a strong foundation for maintaining progress. Even if you eventually choose surgery or medication, solid lifestyle patterns make the entire journey smoother and more effective.
Weight Loss Surgery vs GLP-1s: How Do They Compare?
Weight loss surgery and GLP-1 or GIP medications work in very different ways, and understanding those differences helps you decide which approach fits your needs right now.
Surgery changes the stomach or intestines to influence appetite, portions, and hormone signalling, which often leads to larger and more durable weight loss.
GLP-1s work by slowing stomach emptying, reducing appetite, and improving blood sugar regulation. They tend to be most effective for people with lower BMI ranges, individuals who want a non-surgical option, or those who need additional support after surgery.
Surgery offers a strong metabolic impact and can rapidly improve conditions like type 2 diabetes or sleep apnea, while GLP-1s offer flexibility, fewer upfront risks, and easier access.
Many people use both strategically. For example, someone might start with GLP-1s to lower surgical risk or use them after surgery to help maintain long-term results. Each option brings meaningful benefits, and the best choice depends on your medical history, goals, and comfort level.

Feature | Weight Loss Surgery | GLP-1 / GIP Medications |
Typical Weight Loss | 50–80% excess weight loss depending on procedure | 10–20% total body weight loss on average |
Speed of Results | Fastest changes in the first 3–6 months | Gradual, increasing over several months |
Durability | Often long-term with strong follow-through | Benefits last only while medications are continued |
Metabolic Impact | Significant effects on hormones and blood sugar | Strong improvement in appetite and glucose control |
Best For | Higher BMI ranges, severe metabolic disease | Lower BMI ranges or those not ready for surgery |
Risks | Surgical risks, nutrient deficiencies, and recovery time | GI side effects, cost, and long-term access issues |
Cost | One-time major cost, often insurance-covered | Ongoing monthly costs, often not covered |
Reversibility | Permanent anatomical changes | Fully reversible by stopping treatment |
Role Together | Surgery as the primary tool, with medications for fine-tuning or maintenance | Medications before or after surgery to support results |
How to Find a High-Quality Program
Choosing the right bariatric program can make a major difference in your safety, confidence, and long-term results. These traits help you identify programs that offer strong support, reliable outcomes, and a team that puts your health first.
1. Accreditation and High Surgical Volume
Accreditation shows that a program meets strict standards for safety, quality, and patient care. High surgical volume means the team performs these procedures regularly, which often results in smoother surgeries and fewer complications.
Programs with accreditation usually have well-developed protocols for emergencies, anaesthesia, and postoperative care. High-volume centres also tend to stay current with updated techniques and evidence-based practices.
When you meet with a surgeon, ask how many procedures they perform each year and whether the program holds recognised accreditation. This helps you feel confident that your care is built on experience and consistent quality. It’s an easy way to spot programs that take surgical excellence seriously.

2. Clear Outcomes Reporting
Transparency is a sign of a trustworthy bariatric program. High-quality centres readily share their complication rates, readmission data, average weight-loss outcomes, and long-term follow-up statistics. These numbers give you a realistic view of what to expect and help you compare programs side by side.
Some centres publish their data online, while others discuss it during consultations. Look for programs that welcome questions and provide clear explanations rather than vague reassurance.
This openness shows that they track their results carefully and use that information to improve care. When a program is honest about its strengths and areas for growth, it helps you make an informed decision.
3. Multidisciplinary Team
A strong bariatric program doesn’t rely on a single provider. Instead, it brings together surgeons, Registered Dietitians, psychologists, nurses, and sometimes exercise specialists to support every part of the journey. Each professional plays a unique role.
The surgeon focuses on operative safety, the dietitian supports nutrition and behaviour change, and the psychologist helps you navigate emotional adjustments. This well-rounded approach makes your care feel coordinated and personalised.
It also ensures that challenges are caught early and handled by the right expert. Programs with multidisciplinary teams are better equipped to help you build sustainable habits and long-term success.
4. Robust Follow-Up Care
Good follow-up care is just as important as the surgery itself. High-quality programs offer structured check-ins, support groups, online resources, and regular monitoring of lab values.
These appointments help you adjust supplements, troubleshoot food intolerances, and fine-tune your eating patterns. They also give you a space to ask questions and stay accountable.
People who stay connected with their bariatric team often maintain weight loss more effectively and feel more supported emotionally. Look for programs that clearly outline their follow-up schedule, so you know what to expect in the months and years ahead. Consistency makes all the difference.

5. Nutrition-Focused Care
Nutrition is the backbone of long-term bariatric success, and strong programs make it a priority. You should have ongoing access to Registered Dietitians who specialise in bariatric nutrition and understand the unique needs of each procedure.
Dietitians help you build balanced meals, meet protein goals, manage supplements, and create habits that feel realistic. They’re also the ones who guide you through shifting food tolerances or emotional eating patterns that may surface after surgery.
At Berry Street, we can connect you with insurance-covered dietitians so you can get high-quality support without worrying about out-of-pocket costs.
Programs that emphasise nutrition tend to see better long-term outcomes because patients feel supported, informed, and confident in their routines. Steady guidance from a dietitian helps you stay on track and avoid preventable challenges.
6. Access to Mental Health Support
Emotional well-being plays a major role in long-term bariatric success, and high-quality programs recognise this from the start. They include licensed mental health professionals who understand the emotional shifts that can happen before and after surgery.
These specialists help you explore patterns like emotional eating, body image concerns, or stress-related habits. They also provide tools for coping with rapid changes in appetite, energy, and routine.
Support from a Registered Mental Health Dietitian through Berry Street can be especially valuable, since they understand both the emotional landscape and the nutritional demands of bariatric care.
This combined approach helps you connect the dots between mood, food choices, and long-term habits. Programs that prioritise mental health tend to see stronger patient satisfaction and more stable outcomes. It’s a clear sign that the program values your whole health, not just the surgical piece.

7. Personalized Care Plans
Every patient brings a different medical history, lifestyle, personality, and set of goals, and strong programs tailor their recommendations accordingly. Instead of offering a one-size-fits-all approach, they take time to understand your needs and design a plan that fits your life.
This might include tailored nutrition goals, specialised postoperative instructions, or additional medical evaluations. Personalised care plans also adapt over time as your body changes and your goals evolve.
You’ll feel more supported because the plan reflects your specific strengths and challenges. Programs that value personalization are often better at preventing problems early and helping people stay consistent long term. It’s a sign of thoughtful, patient-centered care.
Weight Loss Surgery FAQs
Which surgery is “best” and “safest”?
It depends on your health, goals, and medical history. Sleeve and bypass are the most common because they balance safety and effectiveness.
Do I qualify with my BMI/comorbidities?
Most people qualify at a BMI of 40 or at a BMI of 35–39.9 with a significant medical condition.
How much does it cost without insurance?
It varies widely, but most procedures cost tens of thousands of dollars before insurance or discounts.
What can I eat after surgery?
You’ll follow staged textures and eventually maintain a diet focused on protein, hydration, and nutrient-dense foods.
Can I get pregnant after surgery?
Yes, but waiting 12 to 18 months until weight stabilises is typically recommended.
Will I need vitamin supplements forever?
Most procedures require lifelong supplementation, especially bypass or duodenal switch.
Is ESG or a balloon right for me instead?
They can be good options for lower-BMI individuals or those wanting less invasive choices.
Can surgery resolve my diabetes?
Many people experience improvement or remission, particularly with gastric bypass.
What if I don’t lose enough or regain weight?
Revisions, medications, or renewed behavioural support can help. Early intervention is most effective.

Conclusion
Choosing weight loss surgery is a significant step, and understanding the procedures, expected weight loss, eligibility criteria, costs, preparation, and recovery helps make the process clearer. Many people find that surgery offers meaningful improvements in health, mobility, and daily life when combined with supportive nutrition and behavioural habits.
The long-term picture matters, including follow-up care, potential revisions, non-surgical tools, and selecting a program that provides strong multidisciplinary support.
If you’re ready for guidance that feels personal, practical, and rooted in real expertise, connect with a Registered Dietitian covered by insurance at Berry Street to take your next step.
If you want to learn more, why not check out these articles below: